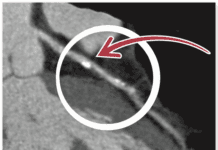
Men who are tall and obese face a higher risk of potentially dangerous blood clots, according to research published in Arteriosclerosis, Thrombosis and Vascular Biology: Journal of the American Heart Association. Obesity is a well-established risk factor for clots in deep veins, especially those in the legs, and for pulmonary embolism, a clot in the blood vessels of the lungs that can result in sudden death or strain on the heart. Together the two conditions are called venous thromboembolism (VTE). Compared with men 57" or shorter and normal-weight men, the age-adjusted risk of VTE was 5.28 times higher in obese and tall men and 2.11 times higher in obese and short men. Researchers noted that the amount of risk conferred by being both tall and obese was comparable to other risk factors for VTE, such as pregnancy and carrying the gene for an inherited predisposition to clotting (known as Factor V Leiden). Because blood must be pumped a longer distance by the calf-muscle group in tall people, there is a higher risk of reduced blood flow in the legs and therefore a greater risk of clotting. This makes it particularly important for tall men to manage their weight and exercise, since height is not a controllable risk factor.
To continue reading this article or issue you must be a paid subscriber.
Sign in