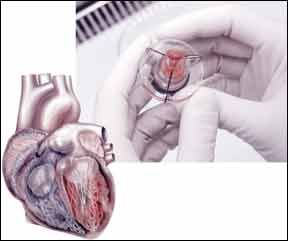
When one of your heart valves needs to be replaced, you have two choices: a mechanical valve or a bioprosthetic valve, made from the heart valves of a pig or cow. Several key factors must be considered when making such a decision, and a recent study suggests that the age of the patient may be among the most important factors. A study presented at the Society of Thoracic Surgeons annual meeting in February found that younger heart valve patients are more likely to survive 10 years if they have a mechanical valve, as opposed to a bioprosthetic valve.
To continue reading this article or issue you must be a paid subscriber.
Sign in