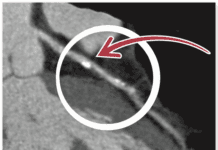
Heart disease remains Americas number one killer, and medical technology is in hot pursuit of ways to diagnose patients earlier and more accurately and treat them less invasively. This has resulted in an explosion of cardiac imaging tests and procedures performed every year. In many instances, there is little doubt these tests save lives. However, all but magnetic resonance imaging (MRI) and some ultrasound-based procedures expose patients to radiation.Patients and physicians alike have growing concerns about the long-term cancer risks from radiation delivered through CT angiography, myocardial perfusion imaging, diagnostic cardiac catheterization, percutaneous coronary procedures and electrophysiology procedures.
To continue reading this article or issue you must be a paid subscriber.
Sign in