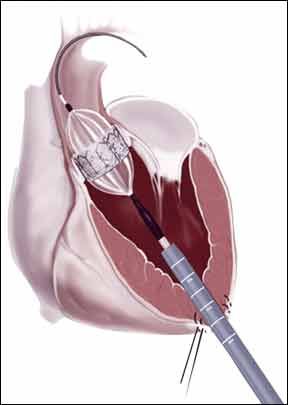
Receiving a new heart valve can be a lifesaving treatment, but its important to understand the limitations and realities of life with a prosthetic valve. A recent study in the Journal of the American College of Cardiology, for example, found that having elevated plasma ratios of two established cholesterol markers can significantly increase the risk of valve degradation in a patient with a bioprosthetic aortic valve. The two markers were apolipoprotein B and A1 (apoB and apoA1). ApoB is a major component of LDL (bad) cholesterol, while apoA1 is a component of HDL (good) cholesterol.
To continue reading this article or issue you must be a paid subscriber.
Sign in