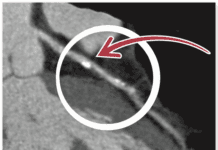
Shedding pounds, especially around your midsection, can help improve your blood vessel function, according to research presented earlier this year at the American Heart Associations Nutrition, Physical Activity and Metabolism Scientific Sessions. The six-month weight-loss study found that the more belly fat participants lost, the better their arteries were able to expand as needed to allow blood to flow more freely. Participants were placed on either a low-carb diet or a low-fat diet. And while both diets resulted in improved vascular function, individuals on the low-carb eating plan lost about 10 pounds more, on average, than those following a low-fat diet.
To continue reading this article or issue you must be a paid subscriber.
Sign in